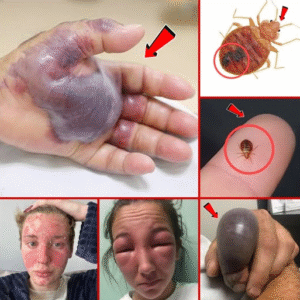
Blackened Hand Highlights the Hidden Dangers of Untreated Infections
In the realm of health and medicine, few images are as startling and instructive as that of a blackened hand—a vivid, almost shocking reminder of what can happen when infections are left untreated. Such cases, though rare, underscore the critical importance of early diagnosis, proper hygiene, and timely medical intervention. While infections are common and often manageable, the progression from a minor cut or wound to a severely infected, discolored, and potentially gangrenous limb illustrates the hidden dangers that can lurk behind what may initially seem trivial.
The story of a blackened hand often begins innocuously. It could start with a small scratch, a burn, or even a puncture wound that goes unnoticed or is considered too minor to warrant medical attention. The skin, our primary barrier against pathogens, may be broken, providing an entry point for bacteria, fungi, or other microorganisms. In healthy individuals, the body’s immune system typically responds effectively, sending white blood cells to fight off infection and triggering inflammation as a protective measure. However, in some cases—particularly when immune function is compromised, hygiene is poor, or an infection is unusually aggressive—the body cannot mount an adequate defense. What begins as a small irritation can rapidly escalate.
Once an infection takes hold, symptoms can progress quietly at first: redness, swelling, warmth, or pain around the affected area. These early signs may be easy to dismiss, particularly in a busy or distracted lifestyle. Over time, however, untreated infections can lead to necrosis—the death of tissue—which is what causes the striking black coloration often associated with severe infections. This blackening is a visual manifestation of serious underlying pathology: the tissue is dying, blood flow has been compromised, and bacteria may be releasing toxins that further damage cells.
One of the most severe forms of infection that can lead to a blackened hand is gangrene. Gangrene can be classified into different types, including dry gangrene, wet gangrene, and gas gangrene, each with distinct characteristics. Dry gangrene occurs when blood flow to a particular area is obstructed, often by conditions such as diabetes or peripheral arterial disease, causing tissue to die slowly and appear dark or black. Wet gangrene, on the other hand, results from a bacterial infection that spreads rapidly, often accompanied by swelling, foul odor, and systemic symptoms such as fever or chills. Gas gangrene, caused by bacteria such as Clostridium perfringens, is particularly aggressive and life-threatening, producing gas bubbles within tissues and often requiring emergency intervention. In all cases, the visual cue of a blackened hand signals a medical emergency.
The dangers of untreated infections extend beyond cosmetic or localized tissue damage. Once bacteria invade deeper tissues, they can enter the bloodstream, leading to sepsis—a systemic inflammatory response that can cause organ failure and death if not promptly treated. Sepsis is a silent killer because it often develops insidiously, beginning with mild symptoms such as fatigue, confusion, or low-grade fever, before rapidly escalating. The presence of a blackened extremity is therefore not just a local concern; it is a potential warning sign of a life-threatening systemic infection.
Several factors can increase the risk of an infection progressing to such severe stages. Chronic medical conditions, such as diabetes, heart disease, or immune disorders, can impair the body’s ability to fight infections. Lifestyle factors, including smoking, poor nutrition, or substance abuse, can further compromise immunity and delay wound healing. Even minor neglect, such as failing to clean a small cut or ignoring early symptoms, can provide the window of opportunity bacteria need to flourish. Social factors also play a role: limited access to healthcare, lack of awareness, and fear of medical costs may prevent individuals from seeking timely treatment, allowing infections to progress unchecked.
Treatment for a severely infected, blackened hand is often complex and urgent. Early-stage infections may respond to antibiotics and wound care, but once tissue necrosis sets in, surgical intervention may be required. Debridement—the surgical removal of dead tissue—is often necessary to prevent the infection from spreading further. In extreme cases, amputation may be the only viable option to save the patient’s life. Postoperative care involves not just infection management but also physical rehabilitation, psychological support, and ongoing monitoring to prevent recurrence. These outcomes highlight how preventable infections can result in lifelong consequences if neglected.
Public awareness and education are critical tools in preventing infections from reaching such severe stages. People should be encouraged to treat even minor cuts, burns, or punctures with care: cleaning the wound thoroughly, applying antiseptics, covering it with a sterile dressing, and monitoring for any signs of infection. Seeking prompt medical advice when symptoms worsen, or when the individual has underlying health conditions, can prevent minor injuries from escalating into severe, blackened necrosis. Awareness campaigns, educational programs, and access to affordable healthcare services can all contribute to reducing the incidence of severe infections.
Medical professionals also emphasize the role of early recognition. Certain visual and systemic cues should never be ignored: discoloration, swelling, persistent pain, foul-smelling discharge, fever, or chills all indicate the potential for a severe infection. Advanced imaging, blood tests, and microbiological cultures can help identify the causative agent and guide effective treatment. Early intervention can often save tissue, preserve function, and prevent life-threatening complications, reinforcing the adage that prompt care is always preferable to delayed treatment.
In addition to immediate care, prevention is key. Vaccinations, proper hygiene, timely management of chronic diseases, and awareness of personal risk factors all play a role in reducing the likelihood of infections escalating to dangerous levels. For individuals with diabetes or compromised circulation, routine monitoring of extremities, proper footwear, and attention to skin integrity can prevent minor injuries from becoming catastrophic. In healthcare settings, strict infection control protocols, sterilization practices, and patient education contribute to lowering the risk of hospital-acquired infections that could result in tissue necrosis.
Ultimately, the image of a blackened hand serves as both a stark warning and a call to action. It reminds us that infections, if ignored, can escalate from something seemingly minor to a medical emergency with profound consequences. The visual impact of blackened tissue captures attention precisely because it signals a breakdown in both the body’s natural defenses and the timely medical intervention that could have prevented the damage. This scenario illustrates a broader truth in medicine: prevention, vigilance, and early action are often far more effective than attempts to manage severe complications after the fact.
In conclusion, the sight of a blackened hand is more than a dramatic visual; it is a testament to the hidden dangers of untreated infections. It encapsulates the progression from a minor injury to tissue necrosis, the potential for systemic infection, and the life-altering consequences that can follow. Through awareness, timely intervention, and preventive care, such outcomes can often be avoided. The story of a blackened hand is thus both cautionary and instructive—a powerful reminder that our health should never be taken for granted, and that even small wounds deserve careful attention. By understanding the risks and acting decisively, we can ensure that infections remain manageable and that the shocking image of a blackened hand remains a rare exception rather than a preventable reality.